Abstract
Background:
There is some evidence indicating that transfusion dependency negatively impact health-related quality of life HRQOL of patients with myelodysplastic syndromes (MDS). However, there is paucity of evidence-based on this relationship across all different disease risk-group categories.
Aims:
The primary objective of this study is to examine whether transfusion dependency has a different impact on HRQOL outcomes (ie. functional wellbeing and symptom burden) by disease risk according to the International Prognostic Scoring System (IPSS).
Methods:
Analysis is based on 669 newly diagnosed MDS patients enrolled in ongoing international prospective observational study. Patients with any IPSS risk score category were consecutively enrolled in 37 centers from nine countries. Patients were invited to participate during one of the first consultations, after confirmed diagnosis of MDS. Multidimensional HRQOL and fatigue outcomes were assessed at baseline (i.e., before treatment) with the well validated European Organization for Research and treatment of Cancer (EORTC) QLQ-C30 and the Functional Assessment of Chronic Illness Therapy ( FACIT) Fatigue questionnaires. Patients were classified as transfusion dependent (TD) or transfusion independent (TI) using the following definition of "transfusion dependency": having received at least one red blood cell transfusion every 8 weeks over a period of 4 months (Malcovati L, et al, J Clin Oncol . 2007; 25: 3503-10). We used proportions, means and medians to describe data, by risk and transfusion-dependence groups. Possible statistically significant differences between groups were assessed by Fisher and Wilcoxon-Mann-Whitney tests according to the type of variable. We also investigated possible clinically meaningful differences according to previously published guidelines.
Results:
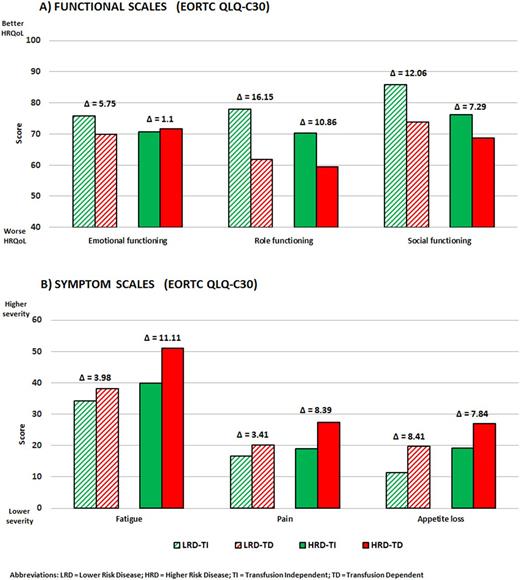
Median age of the entire cohort (N=669) was of 77 years (range 18-96 years) and there were 418 men (62%) and 251 (38%) women. Of the entire cohort, 364 (54%) were classified as IPSS intermediate-2 or high-risk (higher risk disease: HRD) and 305 (46% as IPSS low or intermediate-1 (lower risk disease: LRD). There were: 44(14%) and 261(86%) patients respectively classified TD and TI in the LRD group, while in the HRD group there were 78(21%) and 286 (79%) patients respectively classified as TD and TI. Within LRD and HRD groups, there were no statistically significant differences in age, gender, comorbidity and education level between TD and TI patients. In addition, there were no statistically significant imbalances in the distribution of IPSS risk categories, respectively low and int-1 in LRD patients and int-2 and high-risk in HRD patients, between TD and TI groups. Within LRD, median hemoglobin (Hb) level was 10.2 g/dl and 8.9 g/dl for TI and TD patients and within HRD, median Hb level was 9.5 g/dl and 8.2 g/dl for TI and TD patients respectively. HRQOL profile of TD patients was generally worse than that of TI patients in both LRD and HRD. However, statistically and clinically meaningful differences in key symptoms of fatigue (P=.001, mean difference of 11.1) and pain (P=.002, mean difference of 8.4) were only noted between TD and TI patients within the HRD group. The trend of a fatigue was also confirmed by the FACIT Fatigue scale. Details on mean differences in selected HRQOL scales by disease risk groups (LRD versus HRD) are provided in Figure 1.
Conclusion:
This study suggests that impact of transfusion dependency on HRQOL can be different depending on disease risk at diagnosis with some major impact in fatigue and pain for HRD patients. This data might help physicians to provide more targeted interventions.
Efficace: Incyte: Consultancy; Seattle Genetics: Consultancy; TEVA: Consultancy, Research Funding; Lundbeck: Research Funding; Amgen: Consultancy, Research Funding. Gaidano: AbbVie: Consultancy, Honoraria; Roche: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Janssen: Consultancy, Honoraria. Breccia: TEVA: Speakers Bureau. Platzbecker: Acceleron: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Research Funding; Celgene: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.